Midwifery Leadership: A Global Perspective

In the largest international study of it’s kind, we sought to uncover the qualities that make a midwife a strong leader, and how to cultivate those qualities within the profession. We surveyed hundreds of midwives and nurse-midwives from around the world (76 countries! … predominantly the United Kingdom (UK), Australia, the United States of America (USA), Canada, Uganda, Saudi Arabia, Tanzania, Rwanda, India, and Kenya. The results were enlightening.
What Makes a Strong Midwife Leader?
Midwives identified several key characteristics of strong leadership within their profession. These leaders were described as mediators, dedicated to their work, evidence-based practitioners, effective decision-makers, role models, advocates, visionaries, resilient, empathetic, and compassionate. These traits align with several established leadership styles, including compassionate, transformational, servant, authentic, and situational leadership.
How Can We Foster Strong Midwifery Leadership?
The study also explored ways to enable and strengthen midwifery leadership. Suggestions included investing in a clear professional identity for midwives, increasing societal recognition of the profession, ongoing research, leadership development opportunities, interprofessional collaboration, succession planning, and boosting midwives’ self-efficacy.
Why Does This Matter?

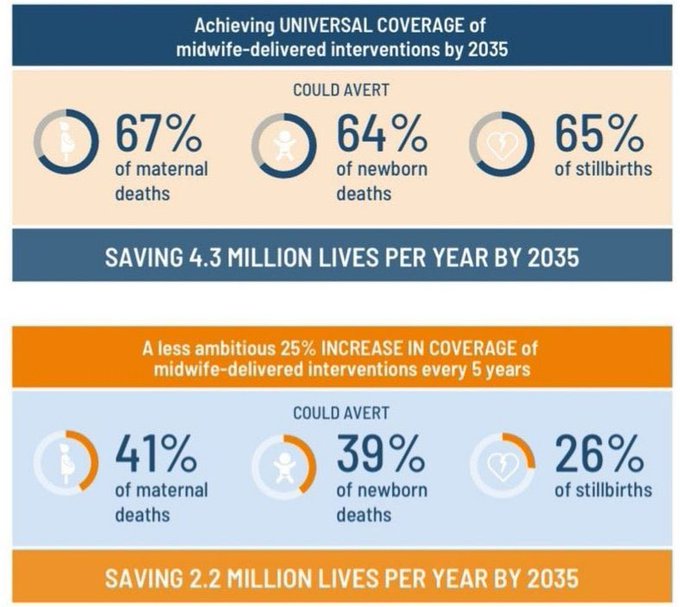
Midwifery is a crucial profession with a significant impact on perinatal health outcomes. By understanding and fostering strong leadership within midwifery, we can elevate the profession and improve perinatal care globally. The findings of this study can inform the development of new leadership models, frameworks, and tools for midwives, ultimately benefiting both practitioners and the families they serve.
The international Confederation of Midwives shared this study in their global newsletter too!
This research sheds light on the complex and multifaceted nature of midwifery leadership, offering valuable insights for midwives, educators, and healthcare organizations seeking to cultivate strong leadership within the profession. By investing in midwifery leadership, we can create a brighter future for midwives and the communities they serve.
How do you thrive as a strong midwifery leader? Do you see strong leadership in others? Do you see this work being used as a framework to support midwifery leadership worldwide? – I would love to hear your thoughts.
Until next time…Look after yourselves and each other
Follow me via @SallyPezaro; The Academic Midwife; TikTok; This blog